Vaccines built around a person’s own DNA have proven effective at beating back cancer, two studies show.
While the studies are small and the results, so far, are limited, the novel approach to cancer care may hint at the personal approach to the treatment of dangerous illnesses that more and more experts are buying into.
The two studies, appearing in the July 5 edition of Nature, highlight the evolving scope of vaccines in the fight against cancer and how, combined with treatments that mobilize the immune system, such innovative therapies may revolutionize the personalization of treatment.
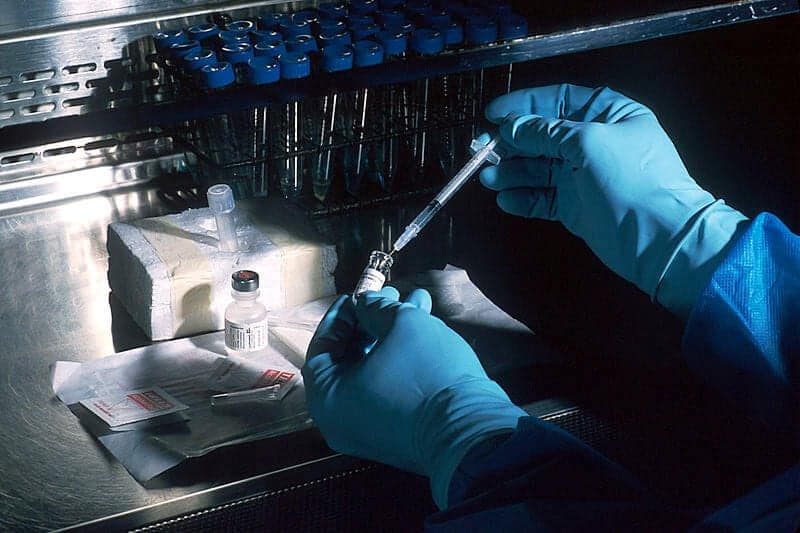
One study, led by Dr. Catherine J. Wu, a researcher at Dana-Farber Cancer Institute and Harvard Medical School, assessed how tapping into a patient’s own genome could help fight cancer.
In the study, researchers targeted substances known as neoantigens, which are distinct genetic markers that appear on a person’s cancer cells, but not on healthy cells. The researchers developed a vaccine that “contained up to 20 neoantigens, derived from an individual patient’s tumor.”
Related: Scientists Disable Cancer’s Ability to Spread Using Tiny Gold Rods
The clinical trial, which found no recurrence of melanoma cancer in four of six patients who received the vaccine, “provides proof-of-principle that a personal vaccine tailored to a patient’s tumor can be produced and generates highly specific responses to that patient’s tumor after vaccination,” reported the researchers.
In the second study, researchers from the University of Mainz in Germany developed a patient-specific vaccine that targeted “10 mutated proteins in each patient.” In patients who received the vaccine after having their melanoma tumors removed and having no visible signs of a tumor, all eight remained cancer-free for more than a year.
“We’ve long recognized in cancer that every patient’s tumor is different. With recent advances in technology, it’s now becoming possible to create a therapy that’s suited to target an individual’s tumor,” report Wu and her colleagues.
Part of the success of the early trials stems from the researchers’ ability to tap into the body’s immune response, which helps in situations where a single drug may prove ineffective.
Related: New Blood Test Aims to Detect Cancer Sooner Than Ever
“We are leveraging the immune system’s natural ability to detect and attack many target antigens, as it does every time we get an infection,” said Wu.
Researchers believe that combining personalized vaccines with a drug that inhibits the PD-1 protein, essentially rousing the immune system to heightened levels of activity, may be most effective.
The medical community is actively engaging in clinical trials involving such therapies, and the road ahead appears to hold vast promise for personalization.
“Future neoantigen vaccine trials will recruit more patients with advanced disease to test the efficacy of the vaccine, take advantage of improved methods for predicting antigen presentation to boost the number of effective neoantigens and test for synergy with checkpoint blockade and other immunotherapeutics,” wrote Wu and her colleagues.
“If successful in subsequent trials, a personal vaccine has the potential to be applied to any cancer that harbors a sufficient numbers of neoantigens for vaccination,” they concluded.
Richard Scott is a health care reporter focusing on health policy and public health. Richard keeps tabs on national health trends from his Philadelphia location and is an active member of the Association of Health Care Journalists.


![How To: ‘Fix’ Crepey Skin [Watch]](https://cdn.vitalupdates.com/wp-content/uploads/2017/05/bhmdad.png)












