Scientists are ramping up their battle against HIV with upcoming large-scale trials using injections and implants to protect vulnerable groups, like gay men and women in Africa, Reuters reported.
In the future, researchers hope to make matchstick-sized implants with slow-release drugs that could offer year-long protection against HIV.
Biopharmaceutical companies with drugs involved in the trials include GlaxoSmithKline, Gilead Sciences and Merck.

The trial continues off the success of Gilead’s daily little blue pill Truvada, a pre-exposure prophylaxis (PrEP), which has proven to be effective at preventing HIV infection during sex.
According to the Centers for Disease Control And Prevention, Truvada can reduce the risk of HIV by as much as 92 percent.
The pill is only effective if people take it every day, but the problem is not many people do. For example, some women in Africa expressed reluctance to take the pill because they feared what their partners or neighbors would think.
Experts hope that the slow-acting injection given in the privacy of a clinic could eliminate this problem. An implant, on the hand, would not only protect against HIV, but could also be combined with contraception.
“The more options there are the better and I think for some individuals injections will be great,” Jean-Michel Molina, professor of infectious diseases at Hospital Saint-Louis in Paris told Reuters. “Now that we know antiretrovirals have great potential to prevent HIV infections, it is time to really assess other ways to deliver these drugs.”
HIV/AIDS continues to be a major health threat both in the U.S. and abroad. As of 2015, 36.7 million people live with HIV/AIDS worldwide, and 1.1 million people died of AIDS-related illnesses, according to the World Health Organization (WHO).
We Don’t Have A Vaccine Yet
GlaxoSmithKline’s majority-owned ViiV Healthcare unit is working with the U.S. government and the Bill and Melinda Gates Foundation in hopes of creating the first injectable PrEP.
They plan on starting a four-year study testing its experimental drug in the Americas and Thailand. Next year, researchers hope to conduct a similar study for women in Africa.
“The holy grail is a vaccine, but we don’t have a vaccine yet,” Myron Cohen of the University of North Carolina at Chapel Hill, who is involved in the ViiV prevention study program told Reuters.
Cohen and his team are also working on another HIV-prevention trial that gives people antibodies through an intravenous drip.
In the meantime, Gilead is in the late stages of a study on their next-generation HIV drug called Descovy, which they believe could be an alternative to Truvada because of its comparatively milder side effects.
Cohen and other HIV experts hope that slow-release drug implants are the future for HIV prevention.
Some Call Truvada A “Party Drug”
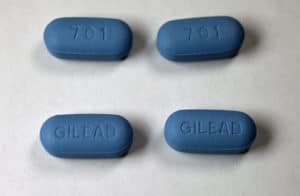
Truvada has caused a debate within the gay community, with some calling the little blue pill a “party drug” that encourages people not to use condoms. Some people also worry that if not taken consistently, Truvada is not effective in staving off HIV.
“You have to be really paranoid about your health to wear a belt and suspenders,” AIDS Healthcare Foundation President Michael Weinstein told the Los Angeles Times in 2014. “If the culture shifts to unprotected sex because of the campaign to promote Truvada, then [HIV] rates will go up.”
Recently, a French government campaign promoting HIV awareness, including Truvada, was under scrutiny from several French mayors, who argued that it diluted the message of “safe sex” and condom use.
But Sheena McCormack of University College London says that many of these concerned activist miss the point.
“Sometimes people can’t see the wood for the trees,” McCormack told Reuters. “The STI that lasts a lifetime and costs governments a lot of money is HIV.”
Danielle Tarasiuk is a multimedia journalist based in Los Angeles. Her work has been published on AllDay.com, Yahoo! Sports, KCET, and NPR-affiliate stations KPCC and KCRW. She’s a proud Sarah Lawrence College and USC Annenberg alumn.


![How To: ‘Fix’ Crepey Skin [Watch]](https://cdn.vitalupdates.com/wp-content/uploads/2017/05/bhmdad.png)












