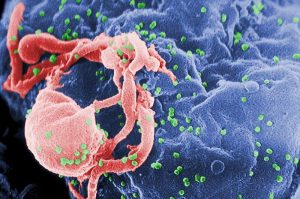
For people with HIV, the evolution of the CRISPR/Cas9 story has offered perhaps one of the realest possibilities for a cure, even as science fiction-sounding as it is.
But now, that sci-fi story has inched another step closer to reality. Researchers at Lewis Katz School of Medicine at Temple University have used CRISPR/Cas9 to edit HIV right out of the genome of infected, “humanized” mice.

The strategy was tested on three different types of mice. These researchers had conducted previous experiments on mice using CRISPR/Cas9 but with less impressive results.
“During acute infection, HIV actively replicates,” said Dr. Kamel Khalili. “With EcoHIV mice, we were able to investigate the ability of the CRISPR/Cas9 strategy to block viral replication and potentially prevent systemic infection.”
According to Temple, 96 percent of HIV was successfully excised from the EcoHIV mice.
CRISPR/Cas9 is a new technology that essentially “edits” the human genome. It can be injected into the body along with a “vector,” or harmless pathogen. This time, the scientists modified the vector to achieve better results. “The AAV-DJ/8 subtype combines multiple serotypes, giving us a broader range of cell targets for the delivery of our CRISPR/Cas9 system,” said Dr. Wenhui Hu.
Related: Scientists May Be Getting Closer to Curing HIV
Last year, CRISPR/Cas9 scientists explained they were running into a problem with HIV mutating and escaping the CRISPR.
“When we sequence the viral RNA of escaped HIV, the surprise is that the majority of the mutations that the virus has are nicely aligned at the site where Cas9 cleaves the DNA, which immediately indicates that these mutations, instead of resulting from the errors of viral reverse transcriptase, are rather introduced by the cellular non-homologous end joining machinery when repairing the broken DNA,” said Dr. Chen Liang, Senior Investigator at the Lady Davis Institute at the Jewish General Hospital and associate professor of Medicine at the McGill University AIDS Centre, in a McGill news release.
“Some mutations are tiny — only a single nucleotide — but the mutation changes the sequence so Cas9 cannot recognize it anymore. Such mutations do no harm to the virus, so these resistant viruses can still replicate,” Liang said.
Related: CRISPR Pills Could Replace Antibiotics
While HIV is a manageable chronic disease, people living with it must take medication for their rest of their lives. The second the medication is stopped, HIV comes out of hiding — from reservoirs where the medication can’t find it — and starts replicating again.
So, what’s the next step in bringing CRISPR/Cas9 to humans with HIV? Testing on monkeys.
“The next stage would be to repeat the study in primates, a more suitable animal model where HIV infection induces disease, in order to further demonstrate elimination of HIV-1 DNA in latently infected T cells and other sanctuary sites for HIV-1, including brain cells,” Khalili said. “Our eventual goal is a clinical trial in human patients.”
A professional journalist nearly 30 years, David Heitz started his career at the Quad-City Times in Davenport, Iowa before moving to Los Angeles. He led the Glendale News-Press to best small daily newspaper in the state (CNPA) as managing editor and also worked as executive news editor of the Press-Telegram. He worked briefly as deputy news editor of the Detroit News before returning to the Quad-Cities, where he has worked as a freelance medical writer since 2012 for several national websites. He recently purchased his childhood home and says he truly is “living the dream.”


![How To: ‘Fix’ Crepey Skin [Watch]](https://cdn.vitalupdates.com/wp-content/uploads/2017/05/bhmdad.png)












