Doctors and scientists who work in the field of HIV seldom use the word “cure.”
That’s because it is going to take a small miracle to wipe the tricky disease off the planet. But startling research published this week in Proceedings of National Academy of Sciences by scientists at the prestigious Scripps Research Institute in La Jolla, Calif. shows yet another way that scientists may someday be able to rid the body of HIV.
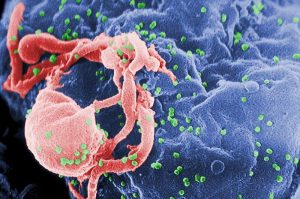
“(Scientists) have found a way to tether HIV-fighting antibodies to immune cells, creating a cell population resistant to the virus,” Scripps explained in a news release. “Their experiments under lab conditions show that these resistant cells can quickly replace diseased cells, potentially curing the disease in a person with HIV.”
City of Hope currently has active clinical trials of gene therapy for AIDS using blood stem cell transplantation. The Scripps research will help inform that work. “The ultimate goal will be the control of HIV in patients with AIDS without the need for other medications,” said Dr. John A. Zala, Director of the Center for Gene Therapy in the Hematological Malignancy and Stem Cells Transplantation Institute at City of Hope.
Related: Campaign Launched to Get More Women Into HIV Heart Health Study
Although HIV is now a manageable disease and people living with it have reached lifespan parity with the uninfected, the medications are costly, must be taken every day and have many side effects.
Although all this research took place in a Petri dish, the methodology of how the scientists did their work is remarkable. “We at TSRI are honored to be able to collaborate with physicians and scientists at City of Hope, whose expertise in transplantation in HIV patients should hopefully allow this therapy to be used in people,” said Dr. Richard Lerner of TSRI.
A Closer Look at the Methodology
So how do scientists tether an antibody to an immune cell?
“The new TSRI technique offers a significant advantage over therapies where antibodies float freely in the bloodstream at a relatively low concentration,” Scripps reported. “Instead, antibodies in the new study hang on to a cell’s surface, blocking HIV from accessing a crucial cell receptor and spreading infection.”
Jia Xie, first author of the study, called it the “neighbor effect,” adding, “You don’t need to have so many molecules on one cell to be effective.”
Related: HIV Patients Have Nearly Double the Heart Attack Risk, Study Says
Before performing their HIV experiments, they first gave cells in a Petri dish a cold. “They used a vector called lentivirus to deliver a new gene to culture human cells,” Scripps reported. “This gene instructed cells to synthesize antibodies that bind with the human cell receptor (ICAM-1) that rhinovirus needs. With the antibodies monopolizing that site, the virus cannot enter the cell to spread infection.”
In the case of HIV, it cannot attach to a cell without a CD4 receptor. The “cold” experiment worked the same with HIV.
“This is really a form of cellular vaccination,” said Lerner.
A professional journalist nearly 30 years, David Heitz started his career at the Quad-City Times in Davenport, Iowa before moving to Los Angeles. He led the Glendale News-Press to best small daily newspaper in the state (CNPA) as managing editor and also worked as executive news editor of the Press-Telegram. He worked briefly as deputy news editor of the Detroit News before returning to the Quad-Cities, where he has worked as a freelance medical writer since 2012 for several national websites. He recently purchased his childhood home and says he truly is “living the dream.”


![How To: ‘Fix’ Crepey Skin [Watch]](https://cdn.vitalupdates.com/wp-content/uploads/2017/05/bhmdad.png)












